Head and Neck
Author
Tieying Hou, MD, PhD
Summary of clinical history
A 53-year-old female with no history of malignancy presented with a two-month history of nasal congestion. CT imaging revealed a 3.8 cm soft tissue mass in the right nasal cavity, extending into the frontal sinus and nasopharynx. One of the differential diagnoses based on radiologic findings is a sinonasal polyp.
Gross findings
The specimen, obtained from a nasal cavity biopsy, consists of multiple tissue fragments measuring between 0.5 cm and 1.5 cm.
Microscopic findings
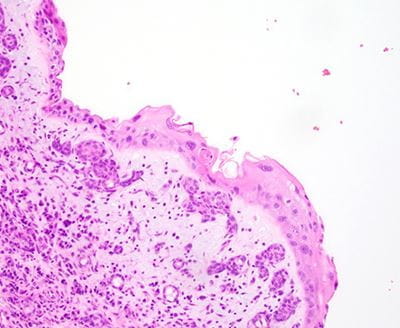
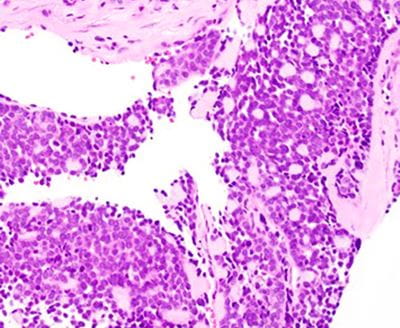
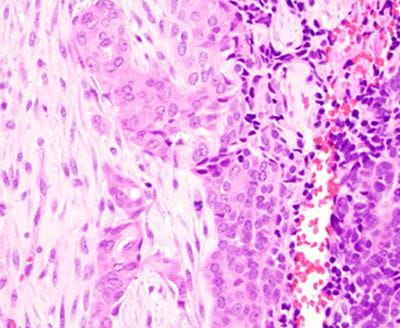
The tumor predominantly grows in the submucosal areas, forming cribriform nests, ductal structures, trabecular arrangements, or solid sheets. The tumor cells are basaloid with scant cytoplasm. Focal areas of squamous differentiation, characterized by eosinophilic cytoplasm, are observed. The overlying squamous mucosa exhibits high-grade dysplasia.
Click any image for a larger version.
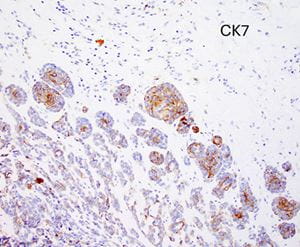
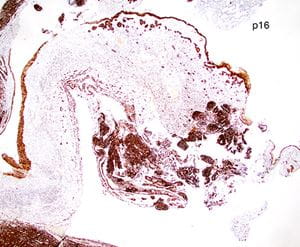
Immunohistochemical findings
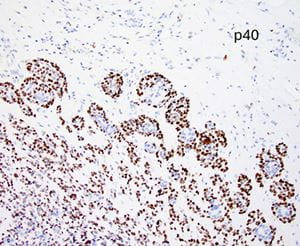
Immunohistochemical staining for CK7 and p40 highlights dual cell populations, identifying ductal and myoepithelial components. P16 shows diffuse block positivity. High-risk HPV genotyping by PCR confirms the presence of HR-HPV types 33 or 58.
Click any image for a larger version.