The Indiana University School of Medicine Department of Psychiatry and the Indiana Family and Social Services Administration, Division of Mental Health and Addiction (DMHA) to conduct a statewide implementation of Multisystemic Therapy (MST®) in youth-serving organizations across Indiana.
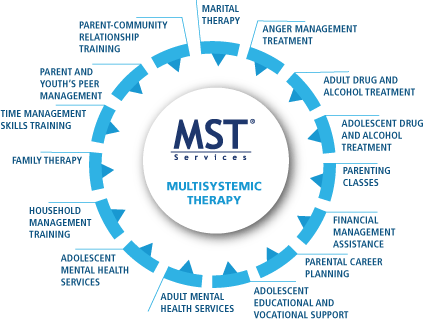
MST is a community and family-focused intervention that has been scientifically proven to transform the lives of troubled youth and their families. MST teams across the state are passionate about serving at-risk youth and are seeking referrals.
Criteria that would make a youth eligible for MST include:
- Youth ages 12-17
- Engaging in aggressive and/or criminal behaviors
- Having problem behaviors at school or are chronically truant
- Using and/or selling substances
- At risk of placement out of the home and/or severe system consequence (e.g., school expulsion or arrest)
- Involvement with the Department of Child Services or juvenile justice systems