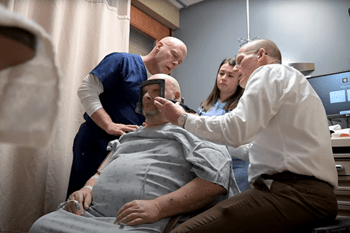
Faculty in the Department of Neurological Surgery at Indiana University School of Medicine perform focal resections, stereotactic laser ablation, responsive neurostimulation, deep brain stimulation and vagal nerve stimulation to treat epilepsy in patients. While surgeons in this specialty currently implant electrodes to localize epileptogenic foci using frame-based and frameless techniques, the department anticipates acquiring the technology to robotically implant electrodes to enhance diagnostic yield. Alongside excellent teams of epileptologists and movement disorder specialists, IU School of Medicine neurosurgeons have helped establish IU Health as a Level 4 Epilepsy Center, the highest possible accreditation by the National Association of Epilepsy Centers as well as a Center of Excellence by the National Parkinson’s Foundation. Faculty provide comprehensive evaluation and management of patients with medically intractable complex partial seizures.
 Neuromodulation Therapies
Neuromodulation Therapies
Faculty in the specialty offer the full range of epilepsy surgery, from open craniotomy for resection to Laser Interstitial Thermal Therapy (LITT), as well as the latest in neuromodulation therapies, including deep brain stimulation, responsive neurostimulation and vagal nerve stimulation. Faculty surgeons also perform procedures part of the StereoElectroEncephaloGraphy (SEEG) program to precisely localize the origin of patients’ seizures and guide planning of subsequent therapeutic operations. These procedures have led to temporal lobectomies, laser ablations and stimulator implants.
 Deep Brain Stimulation and Focused Ultrasound
Deep Brain Stimulation and Focused Ultrasound
Movement disorders, including Parkinson’s disease, essential tremor and dystonia, are treated with a multidisciplinary team approach that uses microelectrode-based deep brain stimulation and ablative procedures. Deep brain stimulation is a minimally invasive surgical treatment that involves placing fine stimulating electrodes into specific areas of the brain that control movement. Each patient’s treatment plan is customized specifically to their health needs and a full range of novel advancements in DBS technology is available. Faculty have contributed to national deep brain stimulation registries, an investigator led trial examining novel indications for deep brain stimulation. Focused ultrasound thalamotomy, a cutting-edge, non-invasive operation, is a treatment for patients experiencing essential tremor who have not responded to medications. Patients are referred to a movement disorder neurologist first to see if focused ultrasound is an appropriate treatment for their condition. If they are a good candidate for the procedure, they’ll next meet with a neurosurgeon to plan out the focused ultrasound thalamotomy. The procedure has no incisions, drilling or burr holes. It instead directs ultrasonic waves to a small part of the brain that is responsible for the tremor. Patients will usually see immediate improvement after multiple rounds of the ultrasonic waves. Throughout the procedure the amount of energy from the ultrasonic waves increases the heat needed to form a lesion to eliminate brain tissue that’s causing the tremor.