INDIANAPOLIS—Researchers from the Indiana Center for Regenerative Medicine and Engineering (ICRME) have identified a new type of cell in the human and mouse body called the vasculogenic fibroblast that provides critical insight into how new blood vessels can be made when needed for treatment.
Blood vessels are created by endothelial cells, but researchers found a different kind of cell, the vasculogenic fibroblast, can also make new blood vessels and achieve blood flow. They describe their findings in a newly published paper in Nature Communications.
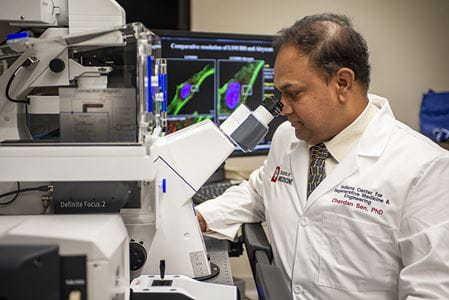
“Ischemic diseases are common and limited by poor blood supply—diabetic wounds are one of them,” said Chandan K Sen, PhD, distinguished professor of surgery, associate vice president of military and applied research at IU School of Medicine and director of the ICRME. “Growing blood vessels to treat ischemic disease and arresting growth of blood vessels to limit tumor growth requires complete understanding of how blood vessels are made in the body. The discovery of vasculogenic fibroblasts unveils a critical piece of the puzzle that would help targeted therapies.”
Researchers observed vasculogenic fibroblasts in human patients. When someone is injured, the body starts developing vasculogenic fibroblasts that make new blood vessels to heal tissue. But in some patients, such as those with diabetes, the ability to make these specialized cells is blunted. In lab models, Sen and the research team used their tissue nanotransfection (TNT) technology for tissue reprogramming to replenish vasculogenic fibroblasts in diabetic tissue. This led to improved blood flow and improved diabetic wound closure.
“Not only did this work identify a cell that has always quietly functioned in the body, but we can use TNT and vasculogenic tissue reprogramming to make these cells and rescue tissues affected by poor blood supply,” Sen said.
TNT and regenerative medicine, which seeks to replace or regenerate human cells, tissue and organs, is a growing industry around the world and in Indiana. According to MarketWatch, the TNT market was valued at $2.07 billion in 2020 and is expected to increase to $7.06 billion by 2028 due to an increase in skin diseases, chronic diseases and trauma emergencies as well as an increased consciousness of successful tissue engineering programs.
“In less than a second, the TNT nanochip can deliver just one anti-sense oligonucleotide to the skin and convert cells into vasculogenic cells,” Sen said. “This innovative technology is continuing to show promise in providing simple and effective treatment for many different health concerns in many different situations.”
Along with Sen, study authors from Indiana University include Subhadip Ghatak, PhD, Kanhaiya Singh, PhD, Ahmed Safwat Abouhashem, Manishekhar Kumar, PhD, Mohamed El Masry, PhD, MD, Sujit K. Mohanty, PhD, Ravichand Palakurti, PhD, Yashika Rustagi, Saba Tabasum, Dolly K. Khona, Savita Khanna, PhD, Sedat Kacar, PhD, Rajneesh Srivastava, PhD, Pramod Bhasme, PhD, Sumit S. Verma, PhD, Edward Hernandez, MD, Anu Sharma, PhD, Diamond Reese, Priyanka Verma, Nandini Ghosh, Mahadeo Gorain, Jun Wan, PhD, Sheng Liu, PhD, Yunlong Liu, PhD, Surya C. Gnyawali, PhD, Sashwati Roy, PhD, and Mervin Yoder, MD. The study also included authors from The Ohio State University. This work was sponsored by a grant from the National Institutes of Health.
About IU School of Medicine
IU School of Medicine is the largest medical school in the U.S. and is annually ranked among the top medical schools in the nation by U.S. News & World Report. The school offers high-quality medical education, access to leading medical research and rich campus life in nine Indiana cities, including rural and urban locations consistently recognized for livability.