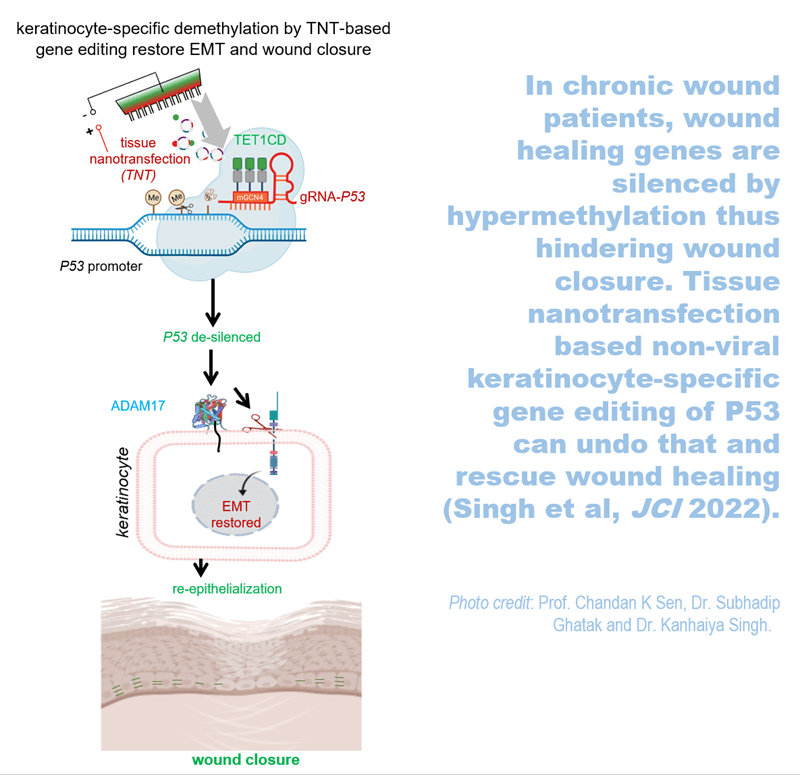
INDIANAPOLIS – The Indiana Center for Regenerative Medicine and Engineering (ICRME) at Indiana University School of Medicine is home to tissue nanotransfection (TNT) regenerative medicine technology that achieves functional tissue reprogramming in the live body. Last year, ICRME researchers published on how to manufacture the TNT 2.0 silicon chip hardware in Nature Protocol. Now, their research demonstrates for the first time that TNT can serve as a non-viral, topical, gene-editing delivery device.
TNT is a minimally invasive device that can reprogram tissue function in the live body by applying pulses of harmless, electric sparks to deliver specific genes of interest to the skin.
“TNT-based delivery can achieve cell-specific gene editing,” said corresponding author Chandan K. Sen, PhD, the J. Stanley Battersby Chair and distinguished professor of surgery, director of the ICRME at IU School of Medicine and executive director of the Indiana University Health Comprehensive Wound Care Center. “Your skin has thousands of genes and in chronic wounds many key genes are silenced by DNA methylation. TNT-based gene editing technology can remove that barrier.”
In this study, genome-wide methylation was observed in the chronic wound tissue of patients. This was reproduced in an experimental murine model. TNT-based, cell-specific gene editing rescued wound healing. Results were published recently in the Journal of Clinical Investigation.

Previous TNT application studies reported on the rescue of injured legs, diabetic neuropathy, crushed nerve and the stroke-affected brain. This is the first time promoter methylation of genes is recognized as a critical barrier to wound healing. In this study, ICRME investigators found that P53 methylation and gene silencing as a critical barrier to cutaneous wound epithelial-to-mesenchymal transition (EMT), a mechanism that is necessary to close skin wounds. TNT based non-viral keratinocyte-specific demethylation of P53 gene rescued EMT and achieved wound closure.
Chronic wounds can result in serious and sometimes life-threatening complications from an abundance of dying and necrotic tissue, such as cellulitis, lower-extremity amputation and sepsis. Treating chronic wounds is estimated to cost the United States health care system $28 billion annually, which amplifies the need to test novel treatments to prevent amputation, save lives and lower health care costs.
“Inspired by observations in chronic wound patients, this work has achieved an important milestone highlighting the need to de-silence genes at the wound-site,” said first author Kanhaiya Singh, PhD, assistant professor of surgery and an investigator at the ICRME.
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases, the U.S. Department of Defense and the Lilly Endowment INCITE program.
###
IU School of Medicine is the largest medical school in the U.S. and is annually ranked among the top medical schools in the nation by U.S. News & World Report. The school offers high-quality medical education, access to leading medical research and rich campus life in nine Indiana cities, including rural and urban locations consistently recognized for livability.