A study co-led by Indiana University School of Medicine researchers points to a promising new strategy for treating myelodysplastic syndromes, a group of age-related blood disorders that can lead to leukemia. Their findings were recently published in Blood.
By investigating the role inflammation plays in myelodysplastic syndromes, the researchers discovered that blocking certain inflammatory signals in the bone marrow may improve the effectiveness of current treatment options. This is particularly beneficial for older adults who are most commonly affected by the blood disorders.
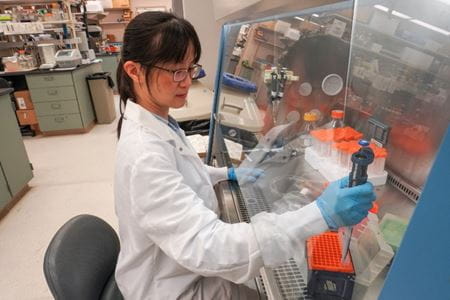
“Current treatments often fail to eliminate the abnormal blood cells found in myelodysplastic syndromes,” said Tzu-Chieh (Kate) Ho, PhD, assistant research professor of pediatrics at the IU School of Medicine and a co-author of the study. “This can lead to disease progression, poor survival and, in many cases, transformation into acute leukemia.”
Myelodysplastic syndromes are driven by dysfunctional hematopoietic stem and progenitor cells, which normally reside in the bone marrow and are responsible for producing all types of blood cells. When abnormal hematopoietic stem and progenitor cells grow, they crowd out healthy blood cells, increasing the risk for other serious blood disorders.
The researchers found increased levels of two inflammation-related molecules — soluble IL-1 receptor 1 (sIL-1R1) and interleukin-18 (IL-18) — in the bone marrow plasma of patients with myelodysplastic syndromes. These markers suggest that inflammatory pathways related to these molecules may be supporting the growth and survival of defective blood cells. Using mouse models, the scientists showed that stopping these inflammatory signals reduced the number of disease-causing cells and also restored the healthy function of the bone marrow’s supportive cells.
“What’s most exciting about this study is that we were able to both reduce the cancer-driving cells and restore healthy function in the bone marrow by blocking certain inflammatory signals,” said Ho. “We also used an age-appropriate model to better reflect how this disease appears in older patients, which makes our findings more relevant for future clinical studies.”
Ho said the findings may pave the way for combining anti-inflammatory strategies with existing treatments to improve patient outcomes for other age-related blood disorders. She expects future studies will validate the results in human myelodysplastic syndrome samples and help identify patient subgroups most likely to benefit from targeted, personalized therapies.