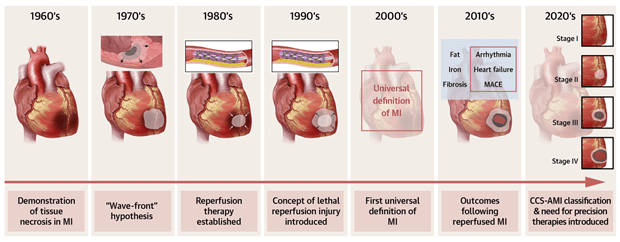
World-renowned researchers who attended the Krannert Biennial hosted by the Krannert Cardiovascular Research Center at Indiana University School of Medicine in May 2023, agree that what happens to the heart muscle after a heart attack is just as critical as to how clinicians treat heart attacks as they happen. They co-authored a State-of-the-Art Review article published in JACC: Advances today on reperfused myocardial infarction (MI), the chief theme of the two-day conference that took a deep dive into damage caused by heart attacks, that cause red blood vessels to rupture and leak into the myocardium.
While one-year mortality after a heart attack has decreased over the past several decades, researchers note, 30% of heart attack patients may still be diagnosed with heart failure after one year. Researchers now are looking at myocardial tissue damage for answers — and potential therapies.
“Not all reperfused myocardial infarctions are the same,” said lead author Rohan Dharmakumar, PhD, executive director of the Krannert Cardiovascular Research Center and vice chair of research for the Department of Radiology and Imaging Sciences at the IU School of Medicine. “From the standpoint of outcomes, it is not only that the size of the MIs that matter, but also whether the microvasculature of the infarcted myocardium remains intact or becomes injured as part of reperfusion therapy.”
Primary percutaneous coronary intervention, also known as PCI, is often used to restore blood flow from a blocked artery, but in turn, can by itself cause injury to the heart muscle. Currently, it is the standard of care for treating ST-segment elevation myocardial infarction or STEMI, a more serious type of heart attack. STEMI occurs when there is a total blockage to the heart’s blood supply in the arteries that needs to be restored immediately. The sooner blood flow can be restored, the greater the chance to prevent permanent heart muscle damage — or at least minimize the injury.
“The JACC Advances article provides the back story to decades of STEMI and reperfusion injury research that led to the development of the four-stage classification of heart attacks established by the Canadian Cardiovascular Society in 2023,” said Andreas Kumar, MD, cardiologist and the immediate past president of the Canadian Society for Cardiovascular Magnetic Resonance Imaging. “These stages are based on severity of tissue damage and can help clinicians determine the risk of heart failure and chance of survival based on the stage.”
 Conceived by Kumar and Dharmakumar, and developed together with an expert panel of cardiovascular specialists from Canada, the classifications include:
Conceived by Kumar and Dharmakumar, and developed together with an expert panel of cardiovascular specialists from Canada, the classifications include:
- Aborted MI
- Acute MI with heart muscle necrosis
- Acute MI with heart muscle necrosis and microvascular obstruction
- Acute MI with heart muscle necrosis and intramyocardial hemorrhage
To prevent a major adverse cardiac event or MACE, post-MI therapies need to address the tissue damage that impacts the pathophysiology, the panel concluded. Severe muscle damage can lead to iron-mediated inflammatory activity and the increased likelihood of MACE.
Timothy D. Henry, MD, an interventional cardiologist with The Christ Hospital Health Network, said half of the people with microvascular injury are more likely to get heart failure and die.
“It’s really important to know whether patients have microvascular injury including hemorrhage, so we can treat them right then,” Henry said.
Researchers here are calling for early risk stratification of heart attack patients, post-PCI, to reduce chances of heart failure. They are investigating novel therapies such as iron chelation therapy, hypothermia and supersaturated oxygen, to potentially improve microvascular perfusion, reduce infarct size and minimize major adverse cardiovascular outcomes following a heart attack. They also write that artificial intelligence may facilitate the prediction heart muscle damage with more accuracy, and direct potential interventions for patients with CCS Stage 4.
Co-author Robert Kloner, MD, PhD, professor of medicine at the Keck School of Medicine at USC and chief science officer at Huntington Medical Research Institutes, said that magnetic resonance has allowed researchers to visualize microvascular obstruction (MVO) and that the classification of myocardial infarction provides an incentive to pursue new targets of microvascular damage.
“Besides myocardial necrosis, myocardial cell death, we now have another target,” Kloner said. “We now have a target of the small blood vessels in the heart. That is a target that we need to focus on. If we can prevent microvascular damage, we might get better healing of the myocardial infarcts, stronger scars, less dilatation of the left ventricle, better function of the left ventricle, less heart failure and maybe less death.”
Co-author Edward T. A. Fry, MD, chair of the Ascension Health Cardiovascular Service Line and past president of the American College of Cardiology, said this JACC: Advances manuscript provides strong scientific basis for increased clinical awareness regarding hemorrhagic infarct and its translation into further risk stratification for early and late adverse events.
“There is certainly strong evidence to suggest incorporating more targeted use of cardiac MRI in a significant number of post MI patients, specifically suspected of CCS Stages 3 or 4, early in their presenting hospitalization,” Fry said.
Co-author Ankur Kalra, MD, MSc, an interventional cardiologist at Franciscan Health and the incoming division chief of cardiology at SUNY Upstate Medical University Hospital in Syracuse, New York agrees.
“The CCS classification will be an important consideration for the care team to guide early and late post MI care to reduce later risk of heart failure, sudden death, readmission and morbidity,” Kalra said.
New frontier of diagnostics
Thanks to advances in imaging within the last 20 years, cardiovascular researchers have experienced a deeper understanding of reperfused myocardial injury, which have helped them assess the compositional, structural and functional changes to the heart over time. Microvascular injury, for example, is best recognized using advanced imaging for diagnosis.
“Stage 4, or acute myocardial infarction, with intramyocardial hemorrhage warrants the use of cardiac magnetic resonance, to sufficiently quantify the extent of heart damage,” Dharmakumar said. “However, new diagnostic tools are needed in other regions of the country and world, where cardiac MRI is not available.”
Kumar further explains that it is impractical to rely on cardiac catheterization alone to document microvascular injury in patients.
“As safer contrast agents are introduced, perfusion echocardiography could become a standard in recognizing microvascular damage in heart attack patients in the future,” Kumar said.
Fry points out the role of cardiac MRI does introduce more challenges.
“The increased role for early and longitudinal cardiac MRI will pose challenges with respect to access, resource availability and service rationalization, especially in rural and underserved communities,” Fry said. “Centralization of the sophisticated reading and post processing capabilities to appropriately identify these patients may help to close these health equity gaps.”
Keyur Vora, MD, MS, a cardiologist and co-author of the manuscript, suggests pathophysiology may help.
“Blood biomarkers could bridge the gap in identifying acute heart attack patients with microvascular injury and refine clinical trial stratification for targeted therapies, but further exploration is needed,” Vora said.
Where to next?
With more broad adoption of the CCS classification of acute myocardial infarction, researchers say investigators can introduce more precision into their clinical trial designs by pinpointing when an intervention might be most effective, so it does not lead to further myocardial injury. Real-time data may also assist in assigning patients to specific treatment arms according to their severity of tissue damage.
“The goals of giving these adjunctive therapies in ischemia reperfusion models is one, to reduce the amount of myocardial cell death, and two, to reduce the amount of damage to the microvasculature, which will also then reduce the amount of hemorrhage,” Kloner said.
He said more work needs to be done to reduce infarct size and microvascular injury, which will hopefully result in better survival and less heart failure.
“There needs to be a lot more education for clinicians about no reflow and about microvascular injury,” Kloner said. “Those that know about it take it seriously. But I think a lot of clinicians are not aware of it as much as they should be.”
While microvascular injury research is gaining momentum, Kloner said there is a lot of interest in ischemic reperfusion damage and the Canadian Cardiovascular Society Acute MI classification and that these developments should incentivize cardiovascular researchers to continue their quest for new interventions.