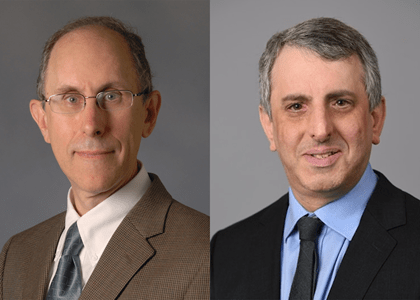
When someone embarks on a career in science, what seems like a straight path often detours into unexpected discoveries. That’s the story of two Indiana University School of Medicine faculty recently elected as 2024 fellows of the American Association for the Advancement of Science (AAAS).
Elliot Androphy, MD, is a dermatologist whose research discoveries led to a biotech startup in human papillomavirus therapeutics and, surprisingly, to the first FDA-approved treatment for the No. 1 genetic cause of infant deaths. Mark H. Kaplan, PhD, is an immunologist who launched IU’s research program in pediatric allergic diseases; he’s now trying to eliminate the risk of death from peanut allergies.
Both scientists also work in cancer research as members of the IU Melvin and Bren Simon Comprehensive Cancer Center. Their discoveries in microbiology and immunology have led them into unexpected fields and promising treatments for multiple diseases.
“You can’t develop a therapy or drug if you don’t have the foundational knowledge,” Kaplan explained. “The therapy discovery is what’s really exciting to the public, but all of the therapies that have come out in the last 10 years that have been really revolutionary in treating cancer are all based on foundational work that was done 15 or 20 years ago.”
“That’s the power of molecular biology and scientific curiosity,” added Androphy.
Elliot Androphy, MD: Quest to end HPV cancer deaths
How did a dermatologist end up discovering a therapy for spinal muscular atrophy (SMA), an inherited neurological disease affecting infants?
“It was quite a coincidence from the papillomavirus research,” said Androphy, a professor of dermatology, of microbiology and immunology, and of anatomy, cell biology and physiology, referencing his primary work in HPV. “What do I know about complex systems of nerves and brain and spinal cord and muscles? I’m not a neurologist or neuroscientist, but we ended up making some very important discoveries in spinal muscular atrophy that led to the first FDA-approved treatment.”
It turns out the same gene his lab was cloning for papillomavirus research was also linked to spinal muscular atrophy.
“Dr. Androphy has made seminal contributions characterizing the molecular defect in the SMN gene that results in the devastating disorder called spinal muscular atrophy and which has now led to new treatments that can dramatically change the outcome for these patients,” said Tatiana Foroud, PhD, executive associate dean for research affairs at the IU School of Medicine.
Now Androphy would like to see that kind of success in his original area of interest — HPV, the leading cause of cervical and oral cancers. Despite the great efficacy of the HPV vaccine, which prevents new infections, it does not alter the course for the millions of people already carrying the virus. That’s why Androphy stepped down from his role as chair of the Department of Dermatology — a post he held from 2010-2022 — and co-founded Kovina Therapeutics Inc, a preclinical stage biotech company. He believes his team has the start of a promising drug therapy.
 “The science is fantastic — things are working,” Androphy said. “But to make a successful drug takes an enormous amount of talent and breadth of experience, as well as copious amounts of money. It’s frustrating when you realize tens of millions of people will die from HPV-induced cancers.”
“The science is fantastic — things are working,” Androphy said. “But to make a successful drug takes an enormous amount of talent and breadth of experience, as well as copious amounts of money. It’s frustrating when you realize tens of millions of people will die from HPV-induced cancers.”
Androphy holds 40 patents related to HPV and spinal muscular atrophy and has been continuously funded by the National Institutes of Health for 40 years. He’s also received grants from the IU Innovation and Commercialization Office and other organizations to advance his science over the years.
“We’ve spent five or six million dollars (on HPV), but you need a lot more to discover a drug and move it into a clinical trial,” Androphy said. “It could fail at any stage. This is my pipe dream. Before I retire, I’d like to take this to clinical trials. It would be a nice capstone on my career.”
Mark Kaplan, PhD: Preventing deaths from peanut allergies
How do cells communicate? And what happens when there’s a problem with the “cell phone” signal?
“Cytokines are kind of like the cellphones of the basic cell world,” explained Kaplan, chair of the Department of Microbiology and Immunology, director of basic science at the Brown Center for Immunotherapy and the Nicole Brown Professor of Immunology at the IU School of Medicine. “We’re interested in knowing who’s got a receiver and what do those cells do when they get those calls?”
 The Kaplan Laboratory aims to develop therapies to regulate inflammatory response in asthma, allergies, cancer and autoimmune diseases. Kaplan is a patent holder with over 250 scholarly publications to his credit. His research has been continuously funded by the NIH since 1999, along with funding from several IU sources and private organizations.
The Kaplan Laboratory aims to develop therapies to regulate inflammatory response in asthma, allergies, cancer and autoimmune diseases. Kaplan is a patent holder with over 250 scholarly publications to his credit. His research has been continuously funded by the NIH since 1999, along with funding from several IU sources and private organizations.
“Recently, some of the big discoveries have been in defining this population of T cells in the lung that secretes this cytokine we’re interested in,” Kaplan said. His quest to understand allergic inflammation led him to other areas, including lung tumors. “It’s a good example of how a discovery in one area can lead to a paradigm that can be applied to many different things. Your findings in asthma might apply to other diseases like cancer.”
Now Kaplan has his sights on ending the risk of death from severe peanut allergies. Working with a researcher at the University of Notre Dame, his team developed a molecule that inhibits anaphylactic reaction from peanut exposure. Clinical trials are currently being designed to test this inhibitor in patients.
 “I am delighted to see the recognition of AAAS for the impactful research that Dr. Kaplan has led at the IU School of Medicine for 25 years that has increased our understanding of how groups of T cells contribute to allergic inflammation,” Foroud said.
“I am delighted to see the recognition of AAAS for the impactful research that Dr. Kaplan has led at the IU School of Medicine for 25 years that has increased our understanding of how groups of T cells contribute to allergic inflammation,” Foroud said.
Despite this high honor, Kaplan considers his impact as an educator a greater achievement. He’s trained dozens of PhD students and postdoctoral fellows over the years; many are now colleagues. He’s particularly proud of Nathan Schmidt, PhD, a professor of pediatrics who studies malaria.
“It’s a lot of fun working with younger scientists that come in with enthusiasm and come up with fresh ideas,” Kaplan said. “Seeing them go on and succeed, when they become your colleagues, you know you’ve had a lasting impact — you’ve changed the field because you’ve added scientists to it.”
As medical scientists, Kaplan and Androphy enjoy the intrigue of investigating unexplored territory within the human body. There’s no end to the potential for discovery.
“One of the really exciting things about research is that there are still areas where we don’t know anything,” Kaplan said.