Photo: The Indiana State Department of Health call center is staffed 24/7 to provide guidance from the CDC to healthcare providers and the public.
Authored by Kris Nanagas, MD
The Division of Medical Toxicology is a multidisciplinary group overseeing the Indiana Poison Center outreach to the public and physicians around the state, inpatient toxicology services, educational opportunities, as well as providing subspecialty expertise in pediatric toxicology, pharmicotoxicology, and neurotoxicology. We are a collaborative and collegial group of faculty physicians, PhD’s, pharmacists, fellows, and Specialists in Poison Information (SPIs). COVID has taught us to be forward thinking, nimble, innovative, and change makers.

When COVID-19 first began affecting Indiana, one of our first orders of business for the Division of Medical Toxicology in the Department of Emergency Medicine was to set up a call center on behalf of the Indiana State Department of Health (ISDH) to assist the public in answering questions regarding coronavirus. Adam Overberg, the managing director of the Indiana Poison Center, spearheaded these efforts. We had to manage recruitment, payroll, infrastructure and training in a few short days. As we were already a skilled call center, we were a natural fit for assistance with efforts such as these. Initially, the phone operators worked within the poison center, but as the number of calls grew exponentially, we quickly outgrew our space and moved to the ISDH. We collaborated with several local universities to recruit addition experts to staff the phones including the Schools of Pharmacy at Butler University and Purdue University, Marion University, and several schools at Indiana University. Our own EM faculty, Megan Palmer and Deb Rusk, were instrumental in assisting with our recruiting efforts. We were able to staff up quickly and provide the concerned public with information at an amazingly rapid pace.
With the COVID work restrictions, the Poison Center had to seamlessly move our operations to virtual platforms in order to keep our Specialists in Poison Information (SPIs) available to the deploy the mission of the Poison Center for the state of Indiana. The Poison Center is a 24 hour a day, 7 days a week service. We relied on our Information Technology expert, Mike Mullins, to issue laptops, headsets and configure all of our SPIs to continuously work from home. Our SPIs also required additional COVID specific education early on due the use of medications like hydroxychloroquine and other alleged remedies to treat COVID would result in an increase in toxicity and potentially fatal exposures. Our SPIs would be faced with providing guidance on these and other unfamiliar agents due to media attention given to purported cures. Many poison centers have seen cases of ‘DIY internet purchases of chloroquine/hydroxychloroquine resulting in toxicity/death. Mary Wermuth created the poison center protocol very quickly to anticipate the need, and also presented that topic to educate the EM residency for their grand rounds.”
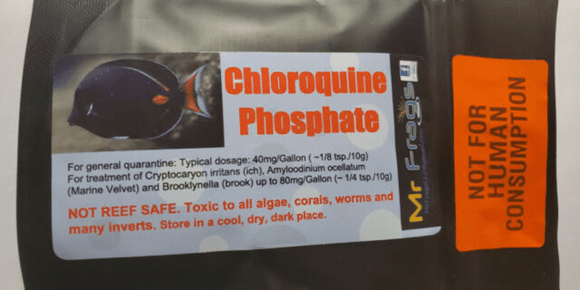
Photo: Lethal Chloroquine Overdose Explained
The majority of our toxicology physicians are trained in Emergency Medicine as their primary specialty, so when the early predictions of the disease model indicated a surge in EDs, we created a back up call schedule that would allow those of us with ED training to do less toxicology call/consults and more shifts if necessary. Laura Tormoehlen (our neurologist/toxicologist) and Blake Froberg (our pediatrician/toxicologist) were very generous with their offers to take the lion’s share of calls if need be, allowing the other four faculty and the two fellows to work in the ED. In order to run the service with a bare minimum of physician coverage, we needed to learn the ins and outs of telehealth, and how to do interprofessional consults via the EMR and alternative forms of communication should it be impossible to go to all the hospitals in person. From reading the news from other countries and cities reporting extraordinary volumes of critically ill patients, we knew there was a possibility that all physicians, regardless of training, would be called to help take care of the masses. For that eventuality, we decided to bring our emeritus faculty out of retirement and create a back-up call system. Jim Mowry, the previous managing director of the poison center, Brent Furbee, the founding father of the medical toxicology service at IU, and Adam Overberg graciously agreed to pitch in. They were able to cover every day of call among the three of them, in the event that all the physicians in the division be redeployed to the front lines.
The resident/student toxicology rotation had to be restructured as well in light of the pandemic. Some departments recalled their residents to be deployed on the hospitalist or ICU services and the medical students were relieved of all their duties as well. We suspended the rotation briefly in order to give the residents a chance to fill in for other services and we learned how to Zoom our didactics and core topics lectures. Currently, we have resumed educational activities but are working to balance learning with safety by minimizing unnecessary contact. We have many fewer rotators than normal- instead of our happy gaggle of 10-12 toxicologists visiting all our hospitals, it is a cozy group of 4-5. Imagine how eerie a feeling it is that we can all fit in one elevator without exceeding the weight limit! Louise Kao reinforces how fellows contributed to the needed changes: “I’d like to recognize the medical toxicology fellows Bryan Ross and Robert Avera for maintaining remote didactic teaching for the rotation. The three of us taught the rotation didactics virtually for about two months”.

Photo: Bob Avera and Mary Wermuth standing in front of an Angel trumpet (a poisonous plant)
While our scholarly activities are waiting in the wings for social distancing to lift, we are eagerly awaiting the ability to start recruiting toxicology patients from the EDs with recreational illicit ingestions again. We have an ongoing project that is working on a rapid test for drug abuse identification that is raring to go once the research coordinators can return to the emergency department for enrollment. So far, we have discovered a staggering array of substances found in our patients- you would be really impressed with the list! We will share it with you...someday.
Lastly, the poison center has been called upon to advise the public on how to safely handle household cleaners. You can read more about the ways the poison center is helping to educate the public in articles from WBST and WishTV.