Indiana University School of Medicine researchers have developed a new microfluidic-based platform to grow and study nerve cells connecting the eye to the brain that are damaged in glaucoma, an eye condition that can lead to vision loss and blindness.
This platform, which the researchers call an “optic nerve on a chip,” models retinal ganglion cells derived from human pluripotent stem cells. The 3D chip allows the team to separate retinal ganglion cells into specific channels to pinpoint where damage from glaucoma occurs. Researchers say this new approach could also be used to study other neurodegenerative disorders like Alzheimer’s disease, Parkinson’s disease and ALS.
The research team, led by Jason Meyer, PhD, the A. Donald Merritt Professor of Medical and Molecular Genetics, and Cátia Gomes, PhD, assistant research professor of medical and molecular genetics, recently published their findings in the journal PNAS. The team also included Kang-Chieh Huang, PhD, co-first author of the study and a PhD graduate of the Department of Biology at IU Indianapolis.
Close to 3 million Americans have glaucoma, and it’s the second-leading cause of blindness worldwide, according to the U.S. Centers for Disease Control and Prevention. Glaucoma damages the optic nerve, formed by retinal ganglion cells, and leads to vision loss and cell death. In neurodegenerative diseases like glaucoma, Meyer said, the damage often starts in the axons, which are long nerve fibers in retinal ganglion cells that carry visual signals from the eye to the brain.
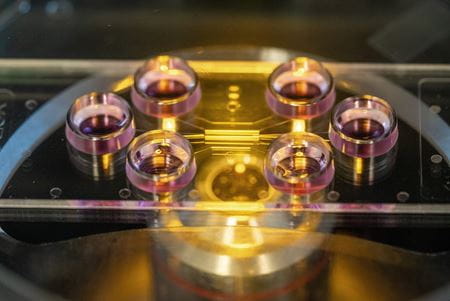
The microfluidic platform is a small, transparent chip made of plastic with tiny channels etched inside to separate different regions of the retinal ganglion cells. The researchers specifically studied how axons are affected by genetic risk factors for glaucoma.
“By creating separate ‘neighborhoods’ on the chip, we can keep different parts of the same cell physically apart while still connected, which allows us to watch how each part behaves,” Meyer said. “This is significant because it gives researchers, for the first time, a realistic way to model how vision-carrying nerve fibers break down in human disease. That knowledge could lead to new ways to protect these cells and make a real difference in slowing or preventing blindness.”
Gomes, co-first author of the paper, said the team found the axons to be vulnerable and show early signs of damage from glaucoma. Past studies examined retinal ganglion cells overall, she added, often overlooking their compartmentalized structure. By separating the axons from the cell body, the team was able to dissect specific mechanisms underlying neurodegeneration.

“This compartmentalized approach not only enhances our ability to model axon-specific disease processes more precisely, but it also holds significant potential as a platform for therapeutic approaches,” Gomes said. “Pharmacological interventions can be applied directly to the axonal region, allowing for the identification and evaluation of strategies that selectively promote axonal survival, outgrowth or regeneration.”
Gomes and Meyer said the chip could be applied to model many conditions where nerve fibers are damaged, such as Alzheimer’s disease, Parkinson’s disease, multiple sclerosis and ALS. Human pluripotent stem cells — used to create retinal ganglion cells in this study — can be developed into any type of cell in the body.
“Anywhere axons are vulnerable, this system could help researchers uncover what goes wrong,” said Meyer, who is the director of stem cell research at the IU School of Medicine’s Stark Neurosciences Research Institute, where he operates his laboratory.
Researchers will next make the model even more complex and realistic by adding other cell types that interact with retinal ganglion cells, such as those involved in neuroinflammation and neurodegeneration, as well as other supporting cell types. They will also try to adapt the model to study the biomechanics of the optic nerve and use the system to test potential drugs that could keep axons healthy and slow or stop vision loss, Meyer said.

This research will run in tandem with other pioneering stem cell studies led by Meyer. In 2024, his lab received $2.2 million from a $46 million multi-institutional award funded by the Advanced Research Projects Agency for Health’s Transplantation of Human Eye Allografts program, part of the U.S. Department of Health and Human Services, to study how using stem cells in a petri dish might stimulate regrowth of nerves between the eye and brain. The goal of the award is to develop treatments to restore vision through whole eye transplantation.
Meyer is also a co-principal investigator of Microphysiological Systems to Advance Precision Medicine for Alzheimer’s Disease and Related Dementias (MAP-AD), a collaborative project led by several IU researchers working to develop stem-cell-based models of the human brain to better understand the underlying causes of Alzheimer’s disease and related dementias.
