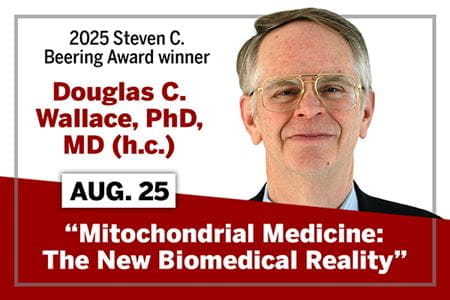
Learn more about Wallace
- Douglas C. Wallace, PhD, faculty profile, Children’s Hospital of Philadelphia Research Institute
- Douglas C. Wallace, PhD, faculty profile, Perelman School of Medicine, University of Pennsylvania
* Disclosure: This article was written by Corie Farnsley with support from Microsoft Copilot. Copilot was used primarily to put complex scientific information into lay terms.